I have worked in Healthcare for more than 30 years – with more than 20 of them as a nurse and the most recent 12 as a nurse in IT. And after all that time, this year was my first HIMSS experience.
Navigating our healthcare system can be difficult for patients and their family members. There are so many stopping points, care providers and transitions – not to mention knowledge dipartites – that make it challenging even for those who are healthy or work in healthcare. These challenges are also present for those entities within the healthcare industry, outside of direct patient care, whose role is to get all of these intricate moving parts to work together, interoperability. Brenda’s story was very real, from the need for rapid assessment and treatment of this communicable disease (Tb) and for it to be expeditiously reported to the correct authorities within her local and state health agencies, to the attention needed for the other clinical findings along the way. Patients, especially those over age 50, typically do not have just one diagnosis managed by one provider. They have multiple diagnosis or family histories that need the attention of multiple providers from varying specialties and settings – each of whom have their own systems, applications, platforms and processes.
Over the years CMS has mandated that disparate organizations promote interoperability to better patient care and the sharing of information across these diverse settings and provider organizations. However, with these directives very little direction or guidance had been provided, leaving vendors and organizations to build their own solutions, often times not fully vetting the results with their peers or those outside of their circle. Therefore continuing the long history of the want for interoperability, but limiting its chance for success.
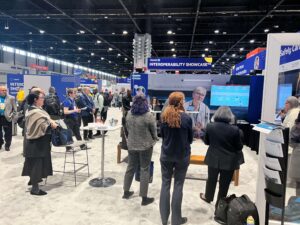
Despite some hurdles our HIMSS Demo team successfully shared real data for Brenda through nine different – and initially unconnected – platforms. Interoperability at its finest. And we did it within a few months, a feat that sometimes takes years. The team working on the “Safely Caring for Those in Need” Showcase was incredibly talented, supportive and motivated. It is amazing what can be done with a few individuals. When given the freedom to work outside some of the normal business silos or organizational constraints. They can break down the barriers and show how interoperability can help improve the care of individuals, inform state and national agencies on greater actionable items for the health and safety of the pubic while following security and compliance protocols.
Konica Minolta’s workflow automation platform played a valuable part in Brenda’s care journey. It took unstructured data from a referral generated by her PCP sent via fax, and converted it into structured data for staff at the nephrology office where she was being referred to edit, validate and send into their EHR, Oracle Health. This expedited Brenda’s access to care, saving staff valuable time, lessening room for documentation errors and connecting disparate data sources. The movement of Brenda’s information in this manner further represents the greater reality that, though there are champions of the use of data and technology in healthcare, a large percentage of clinical information is still captured as unstructured data, and a higher percentage of patient record transactions are still managed by fax. Konica Minolta’s Healthcare services and solutions can be an integral part of facilitating healthcare organizations transformation to having usable discrete data and promoting interoperability within their own organization and to those within the greater community.