Interoperability is an eight-syllable technical term that is often used but can be confusing to many. In its simplest terms it means the ability to connect healthcare’s disparate systems to communicate, exchange and use electronic health data efficiently, accurately and predictably. It’s one of the most important initiatives for the industry today, demonstrated by the abundance of publicly accessible information on the topic. While it’s often perceived as cumbersome and costly, this is a myth. Interoperability is within reach and more accessible than ever.
Understanding Healthcare as a Community
Healthcare is fundamentally a community where a patient’s care is regularly transitioned across different sectors and settings. Care is delivered locally and crosses geo-political boundaries, requiring the seamless sharing of Protected Health Information (PHI). Each transition, regardless of distance, hinges on this exchange.
Exchange Technology
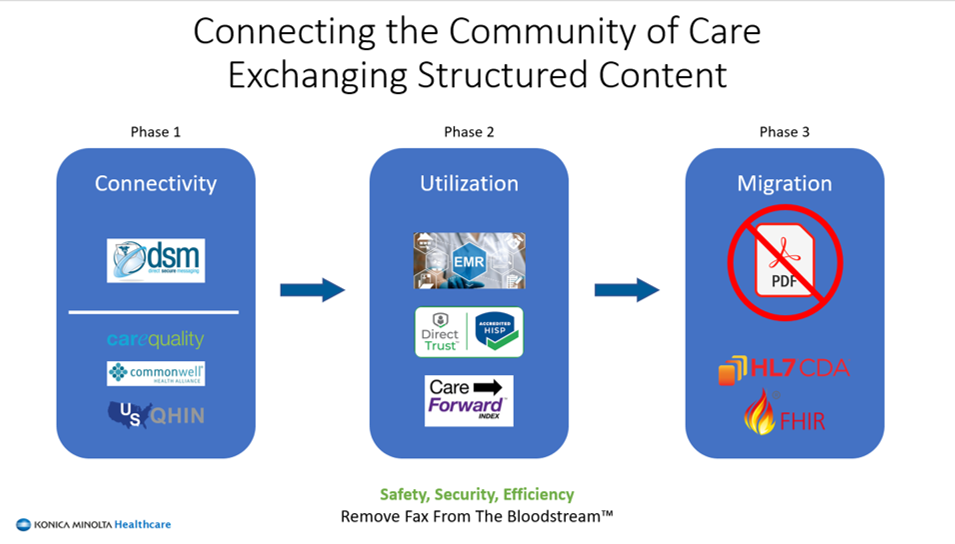
To effectively share PHI, both the sender and the receiver must have compatible technical capabilities, often referred to as the technical stack. Surprisingly, fax remains the most common modality for exchanging PHI among care organizations, despite its flaws. Fax lacks structure, security and identity verification, making it costly and error-prone. There is a better way.
Standards and Workstreams
National industry standards facilitate and normalize the exchange of PHI, regardless of the Electronic Health Record (EHR) system of choice. However, the multitude of exchange modalities and software manufacturers can be overwhelming, leading to decision paralysis. Moreover, many organizations struggle with poorly defined or nonexistent workflows, despite having the technical capabilities.
Simple and Pragmatic Steps to Operationalize
In Summary
Interoperability is not difficult. Start your journey today to reduce costs, save time and mitigate HIPAA-violation risks by connecting with your peers.
Konica Minolta offers proven solutions and services to help care organizations begin, enhance and expand their interoperability initiatives. Learn more here.